Meet today’s case study: ME.
I’ve had foot pain for the past two months (since Feb 18th to be precise). It’s only in the last two weeks that I’ve been able to stand up and walk around more comfortably. I still have a ways to go for my foot to be 100% better.
Actually, “pain” doesn’t acurately describe how my foot feels. It feels like a wet washcloth that hits the floor in a heap and can’t reorganize its self, but also burns and tingles, with patches of numbness.
CT scans (ugh) and ultrasounds reveal nothing “wrong”, nor do I have visible swelling or tissue damage, so I’ve been exploring the biomechanical aspects of this issue, which my team and I suspect is probably neural inflammation.
The scariest thing about my foot situation was that my standard battery of self-assessments, which I regularly use to check in with my biomechanics, are done STANDING.
Suddenly finding myself in a place where I couldn’t stand up, I felt lost and confused about how to assess WHAT was going on with my body, and WHY I’d gotten this way.
Fast forward to March 16th.
My fellow AiM mentor and anatomy nerd pal, Margy Verba, and I decided to do a live gait and movement assessment case study (aka Nerd Out) with me as the case to be studied. We had 10 movement/therapy practitioners join in to observe and participate. It was great fun. And I learned a lot about my body.
Margy knew I had a foot problem, but I didn’t tell her that I still couldn’t stand up, which completely thwarted her plan to have me do standing assessments. Muwhahaha. But Margy’s a pro, and she modified the whole body assessment to be done seated on a stool.
It was brilliant. She even modified the foot motion and windlass assessments to be done sitting down, which I had never done before, and was impressed by the information I got from it depsite being non-weightbearing.
I’d like to share a short (2ish min) clip from the Nerd Out that blew my mind: The spine lateral flexion assessment.
Check it out:
In this clip she is evaluating my ability to hike one side of my pelvis and create lateral flexion (side bending) of my spine.
Can you see which way I struggle to hike my pelvis? And which direction I can’t flex my spine? (if you said, struggle to laterally flex left, and hike pelvis left, you are correct!)
Here’s what blew my mind: My perception of which way I could side bend more easily was not at all aligned with reality.
I thought I could laterally flex my spine left more easily, but turns out I had just found a way of cheating that movement by shifting my ribcage to the right. Can you see it? ‘Cause I couldn’t feel it until Margy pointed it out.
In fact, I’m kind of embarassed to admit it, but I was under the impression that I needed to work on laterally flexing my spine to the RIGHT! Oops.
Take a look at this photo below (a snapshot of me in the loading, or suspension, phase of gait):
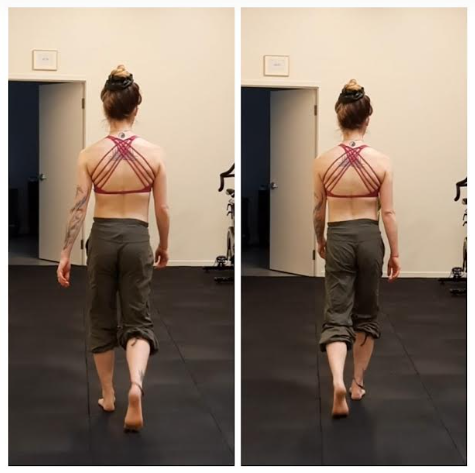
Check out how my spine only laterally flexes to the RIGHT, and never gets left.
Ideally, when we walk, our spine laterally flexes from right to left in the space of one footstep (in less than a second). If we can’t bend equally from right to left, we won’t move as efficiently, and will find alternative strategies to get from one foot to the other. But over time that compensatory strategy may result in things like, oh, I don’t know… Foot pain?
This insight led me to study more deeply the nerves that travel from the lumbar spine and sacrum down into the feet.
Yes, the nerves that keep our feet alive come out of the lumbar spine and sacrum, i.e. the lumbosacral plexus.

Divisions of the femoral nerve, eminating from L2-L4, branch off into the saphenous nerve and plantar nerves, give sensory and motor information to the sole and top of the foot.
Divisions of the sciatic nerve, eminating from L4-S3 branch off into the peroneal nerves, posterior tibial nerves, and calcaneal nerves, whcih give sensory and motor information to the heel and lateral aspect of the foot.
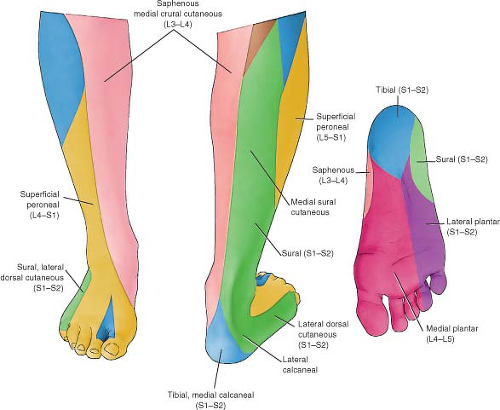
What if the nerves of my right lumbosacral plexus, that go all the way down my leg to innervate my right foot, are being compressed all the time, perpetually smooshed by my inability to get out of a right lateral flexion of my spine?
But me being subjective and blind and thinking I needed MORE right spine lateral flexion, I could have been making the issue worse.
For better or worse, I like to try to figure things out on my own if I can. I’m just glad I asked for help before I continued to jam my spine into a right lateral flexion for a few more months…
This split between perception and reality is completely normal.
When we have pain, we typically experience a loss of proprioception (position sensing). This is why it is so valuable to have a (or a whole team of) support person(s) who can objectively tell you what your body is actually doing, so you don’t make a bigger mess of things, like me.
Getting clear on how my spine was actually moving helped me modify my movement strategies (i.e. stop hurting myself), and things have been steadily improving. It also sparked me to learn more about the lumbosacral plexus and better understand the anatomy involved in my problem.
If we don’t have an awareness of how we are organizing our bodies in movement, we don’t have a chance at understanding how to get ourselves out of the patterns that are keeping us stuck with pain and inefficiencies. Every injury and pain problem is such a wonderful opportunity to learn.
Interested in learning more connections like this? Want help making sense of gait and movement assessments so you can help yourself or your clients/patience with more confidence?
Margy and I plan to do a live Case Study Nerd Out like this every month. Our next one is May 4th, and we’ll be working with a chronic knee issue case (not me this time). If you want to join in, the link to register is HERE.